Oral & Sinus Health: how the oral microbiome effects immunity & overall health

Find out how oral and sinus health are clearly linked to immune support, disease prevention & long-term health.
Did you know that your oral health is related to your ear, nose, and throat health? Were you aware that dental disease is connected to other serious bodily issues such as heart disease, diabetes, and even Alzheimer’s disease? Read on to learn more.
Your mouth is the doorway to your whole body
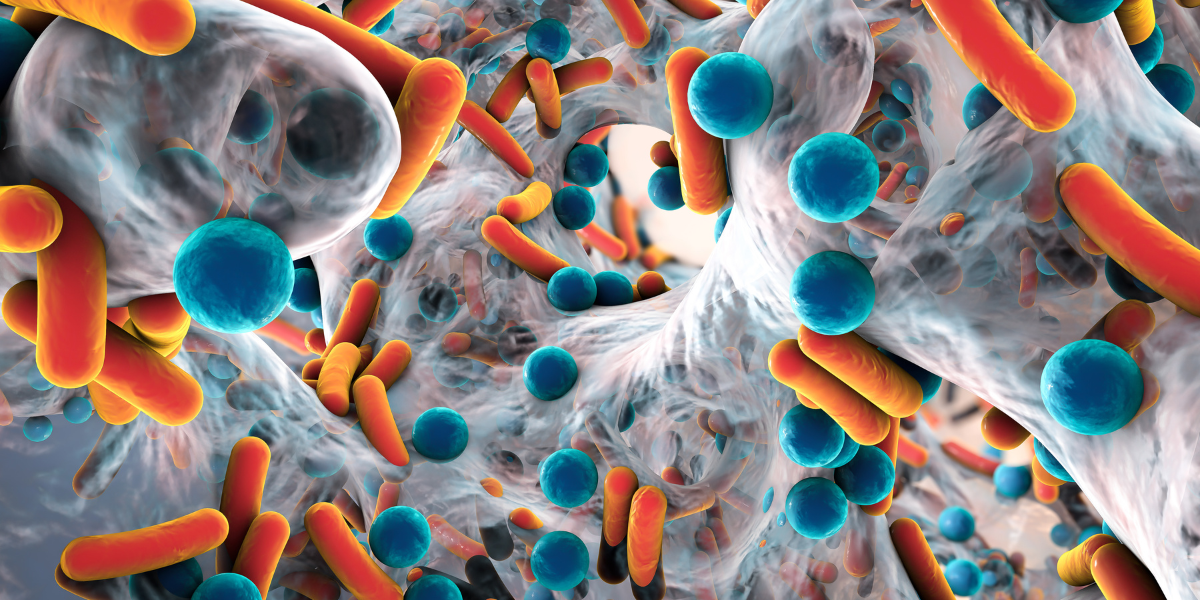
You use your mouth to eat, drink, and even breathe at times. Your mouth is the doorway to your entire body and your health! If your mouth is overpopulated with bad bacteria, not only will you probably have bad breath, but you are also swallowing these bad bacteria all day. Additionally, as you inhale, especially if you are breathing through your mouth, you are introducing the bacteria and other microbes (germs) from your mouth into your airways and potentially into your lungs.
Not all bacteria is bad!
You may have heard that your gut contains good bacteria and bad bacteria. Your mouth does too! The collection of bacteria, viruses, fungi, and protozoa in your mouth is called your oral microbiome, and it has many very important functions [1]. One of the little-discussed jobs of the oral microbiome is supporting your immune system!
Your mouth is the doorway to your health
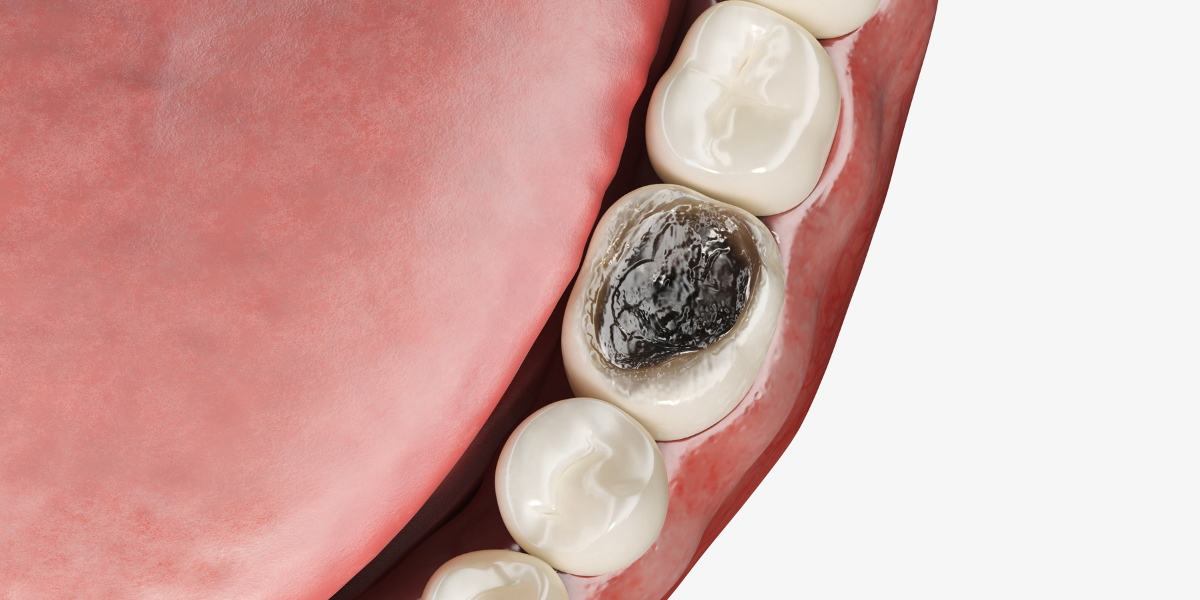
If you think of your mouth as the doorway to your body and your health, you can see that it plays an important role. As mentioned previously, the bacteria in your mouth travels to other areas of your body. Did you know that it can actually enter your bloodstream? From there, it may land in critical organs of your body, such as your heart and brain. In fact, the bacteria known to cause gum disease has been found in the brains of patients with Alzheimer’s disease[3]. There is also a correlation between gum disease and heart disease[4]. In patients with COPD, poor oral health is connected to the increased risk of pneumonia. Poor oral health is known to have connections to other health issues, including diabetes. This is called the oral-systemic link.
Mouth health is connected to ear, nose, and throat health
Studies have shown that certain whole-body (systemic) conditions can alter your oral microbiome[1][5]. This is likely related to inflammatory processes related to disease, which allows bad bacteria to grow in abundance[1][2]. While inflammation can have a negative impact on your health and your microbiome, good bacteria can actually be very beneficial! The bacteria living in your mouth, nose, ears, and throat play an important role in your overall health[2][6]. In fact, your microbiome plays a role in your body’s ability to maintain homeostasis (or stability) in your mouth[6]. Some studies have tested the use of oral probiotics as a way to increase the protective whole-body immunity that vaccines can provide, and have found some success[6].
The oral microbiome affects inflammation
Certain types of good bacteria can actually help to decrease inflammation[1]. This is important because inflammation is elevated in people who are experiencing disease processes such as gum disease (which causes permanent damage to the bone that holds the teeth in), as well as auto-immune diseases. Having a balanced oral microbiome can help to decrease your chances of having inflammation-related disease. Maintaining good oral hygiene at home is one of the easiest and most attainable steps you can take to keep your oral microbiome in check, and to look out for every part of your body!
References
- Idris, A., Hasnain, S. Z., Huat, L. Z., & Koh, D. (2017). Human diseases, immunity and the oral microbiota—Insights gained from metagenomic studies. Oral Science International, 14(2), 27–32. https://doi.org/10.1016/S1348-8643(16)30024-6
- Kaci, G., Goudercourt, D., Dennin, V., Pot, B., Doré, J., Ehrlich, S. D., Renault, P., Blottière, H. M., Daniel, C., & Delorme, C. (2014). Anti-Inflammatory properties of Streptococcus salivarius, a commensal bacterium of the oral cavity and digestive tract. Applied and Environmental Microbiology, 80(3), 928–934. https://doi.org/10.1128/AEM.03133-13
- Liccardo, D., Marzano, F., Carraturo, F., Guida, M., Femminella, G. D., Bencivenga, L., Agrimi, J., Addonizio, A., Melino, I., Valletta, A., Rengo, C., Ferrara, N., Rengo, G., & Cannavo, A. (2020). Potential bidirectional relationship between periodontitis and Alzheimer’s disease. Frontiers in Physiology, 11, 683–683. https://doi.org/10.3389/fphys.2020.00683
- Sanz, M., Marco del Castillo, A., Jepsen, S., Gonzalez-Juanatey, J.R., D’Aiuto, F., Bouchard, P., Chapple, I., Dietrich, T., Gotsman, I., Graziani, F., Herrera, D., Loos, B., Madianos, P., Michel, J.B., Perel, P., Pieske, B., Shapira, L., Shechter, M., Tonetti, M., Vlachopoulos, C., Wimmer, G. (2020). Periodontitis and cardiovascular diseases: Consensus report. Journal of Clinical Periodontology, 47(3), 268–288. https://doi.org/10.1111/jcpe.13189
- Yu J. C., Khodadadi H., Baban B. (2019) Innate immunity and oral microbiome: a personalized, predictive, and preventive approach to the management of oral diseases. EPMA Journal 10(1):43-50. doi: 10.1007/s13167-019-00163-4. PMID: 30984313; PMCID: PMC6459445.
- Zenobia, C., Herpoldt, K.-L., & Freire, M. (2021). Is the oral microbiome a source to enhance mucosal immunity against infectious diseases? Npj Vaccines, 6(1), 80–80. https://doi.org/10.1038/s41541-021-00341-4