The oral-systemic connection: how oral health influences overall health

The mouth is the entry point to the body. Though commonly treated separately by medical & dental providers, there is actually a clear link between the two systems: oral health influencing overall (systemic) health and vice versa. In fact, early signs of systemic diseases are often detected first by dental providers at routine exams.
The mouth is connected to the rest of the body!
While this may seem obvious, you would be surprised how often dental professionals hear patients say things like “Why do you need to know about my medications (or heart health, etc.), I’m just here for a cleaning!” In fact, the mouth plays a very important role in the overall health of the body. Likewise, it is critical for your dental health providers to know your health conditions in order to provide safe health care.
Oral health serves as an indicator for overall health
Dental hygienists and other dental providers are on the front lines for detecting unsuspected health conditions in their patients. For instance, signs of diabetes, pregnancy, or even cancer may be detected in the mouth first, before other diagnostic methods have identified them.
Dental disease can cause systemic disease
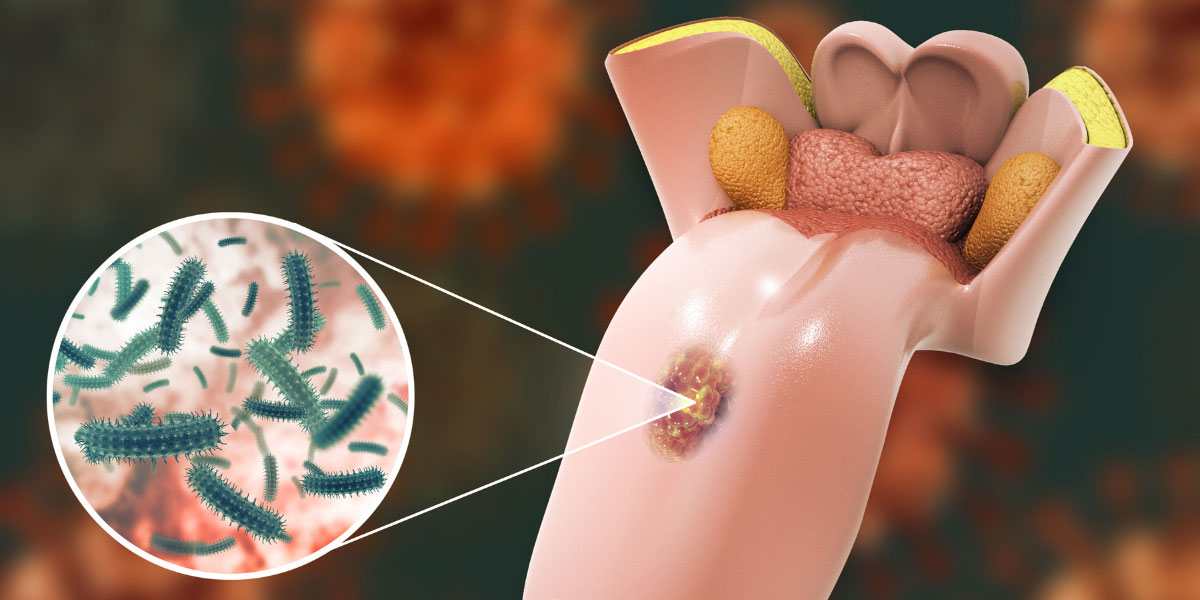
This is key. Studies have shown that dental disease such as periodontitis, also known as gum disease, can increase the risk of other very serious systemic diseases, such as heart disease, stroke, and diabetes. Newer evidence even suggests that chronic periodontitis even plays a role in a debilitating, currently incurable, and sometimes fatal disease: Alzheimer’s[1]. Periodontal disease increases inflammation in the body. Furthermore, the bad bacteria cause periodontal disease can enter the bloodstream and travel to other parts of the body. Periodontal pathogens have been found in arterial plaques associated with heart disease, as well as in the brains of patients with Alzheimer’s disease [1][4]. Additionally, people with periodontal disease are at higher risk of developing diabetes. If someone has uncontrolled periodontal disease, it makes their diabetes more difficult to control [3]. Likewise, if someone has uncontrolled diabetes, they will have a more difficult time getting their periodontal disease under control. This is due to delayed wound healing caused by diabetes, as well as the increased levels of sugar in the blood, which bacteria all over the body feed upon.
Systemic diseases often have oral manifestations
Some people think they are going to the dentist only to have their teeth “scraped” or polished. However, through thorough examination, your dental hygienist or dentist may see red flags that point to other undiagnosed systemic conditions. Cancer or other masses in the body may be detectable through changes in consistency, color, or appearance of the oral tissues, eyes, face, or neck [2]. When a patient’s gums don’t heal as expected after a procedure, it may be a sign of diabetes. Ulcerations in the mouth could point to undiagnosed gastrointestinal issues, such as Crohn’s disease. Viral, bacterial, and fungal illnesses may also be seen in the mouth. Autoimmune diseases such as lupus or rheumatoid arthritis may inhibit salivary flow, which increases the risk of cavities. Dental providers may even be able to identify nutritional deficiencies by looking in your mouth [2]!
Taking care of your mouth is part of taking care of your whole body
By performing good oral hygiene at home and seeing your dental care team at the recommended time interval, you are not only helping to keep your smile in top condition. These oral care visits are essential to maintaining oral health and supporting your whole-body health as well. You can help to lower your body’s inflammatory load and keep disease causing bacteria at bay. You can also rely on your dental health provider to serve as a crucial part of your medical care! They may be the first defense in detecting very serious systemic conditions [2].
References
- Dioguardi, M., Crincoli, V., Laino, L., Alovisi, M., Sovereto, D., Mastrangelo, F., Russo, L. L., & Muzio, L. L. (2020). The role of periodontitis and periodontal bacteria in the onset and progression of Alzheimer’s disease: A systematic review. Journal of Clinical Medicine, 9(2), 495. https://doi.org/10.3390/jcm9020495
- Porter, S., Mercadante, V. & Fedele, S. Oral manifestations of systemic disease. (2017). British Dental Journal 223, 683–691. https://doi.org/10.1038/sj.bdj.2017.884
- Preshaw, P., Bissett, S. (2019) Periodontitis and diabetes. British Dental Journal 227, 577–584. https://doi.org/10.1038/s41415-019-0794-5
- Sanz, M., Marco del Castillo, A., Jepsen, S., Gonzalez-Juanatey, J., D’Aiuto, F., Bouchard, P., Chapple, I., Dietrich, T., Gotsman, I., Graziani, F., Herrera, D., Loos, B., Madianos, P., Michel, J., Perel, P., Pieske, B., Shapira, L., Shechter, M., Tonetti, M., … Wimmer, G. (2020). Periodontitis and cardiovascular diseases: Consensus report. Journal of Clinical Periodontology, 47(3), 268–288. https://doi.org/10.1111/jcpe.1318